TMJ
(58) Demographics of Ohio Licensed Dentists and Treatment Preferences for Temporomandibular Joint Disorders
Thursday, September 12, 2024
2:30 PM - 4:00 PM EDT

Sean W. Noll (he/him/his)
Dental studnet
University of New England College of Dental Medicine
Portland, Maine, United States
Poster Presenter(s)
Disclosure(s):
Sean W. Noll: No financial relationships to disclose
Figure 1: Breakdown of dentists that attended a residency. 414 dentists responded yes and 409 responded no to attending a residency
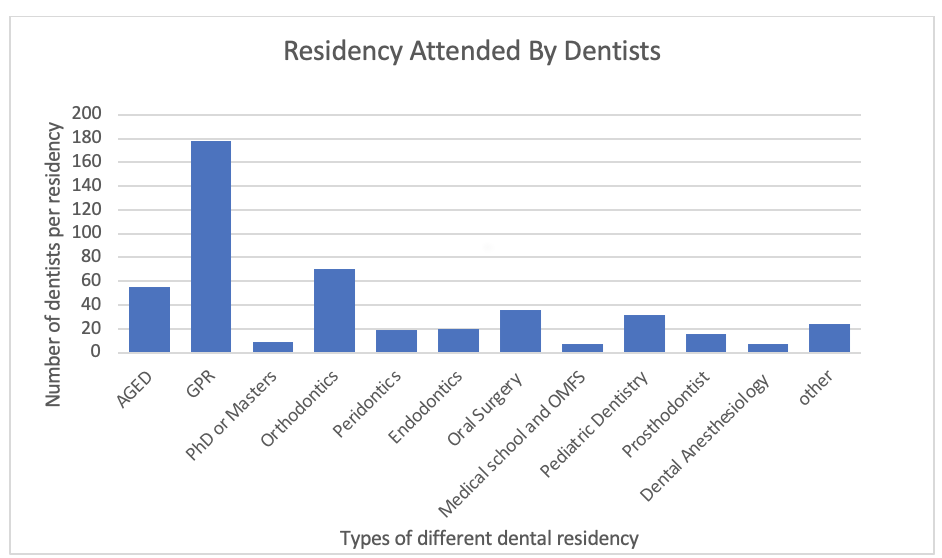
Figure 2. Resources dentists used to stay current in the dental literature.
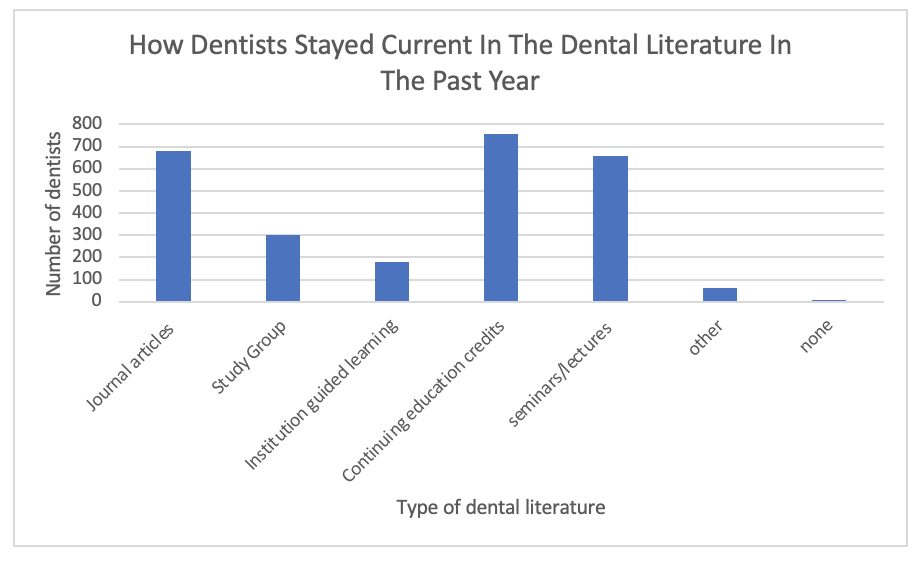
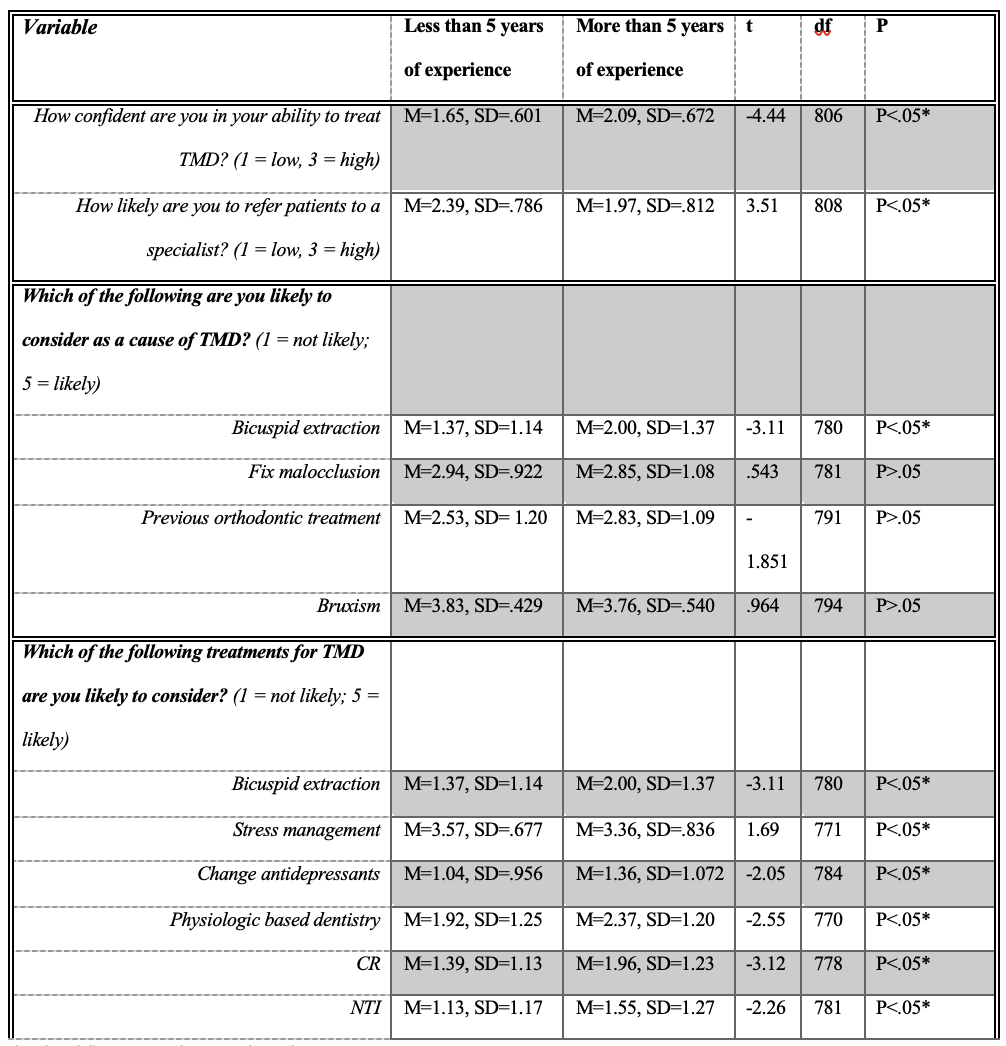
Table 1: Inferential statistics on treatments and causes between dentists working more than 5 years and less than 5 years.