Orthognathic Surgery
OMS and Other Dental Specialists
Session: Oral Abstract Session One
SA1 - Accuracy of Reduced-Size Patient-Specific Cutting Guide and Fixation Plates in Maxillary Orthognathic Surgery
Friday, September 13, 2024
9:20 AM - 9:30 AM EDT
Location: W315B, Orange County Convention Center
.jpg)
Waldemar D. Polido, DDS, PhD, MS
Clinical Professor, Oral and Maxillofacial Surgery
Indiana University Oral and Maxillofacial Surgery
Indianapolis, Indiana
Oral Abstract Presenter(s)
Abstract: The use of VSP, custom cutting guides and PSI in orthognathic surgery is considered today's state-of-the-art. The accuracy of the use of this technology has been proven in recent publications (Jones et al, 2022). However, it is frequently associated with a larger and more invasive surgical approach, in order to achieve a perfect fit of the guide and placement of fixation. The use of minimally or reduced invasiveness concepts in orthognathic surgery is rapidly growing and may bring several advantages over the classic techniques (Al Asseri and Sweden, 2018). The purpose of this study is to assess the accuracy of maxillary repositioning using a reduced-size cutting guide placed along the piriform rim region, through a reduced invasiveness approach for a Le Fort I osteotomy. Our hypothesis is that a cutting guide with reduced dimensions, placed in the anterior maxilla only, allows for accurate repositioning of the maxilla after Le Fort I osteotomy. Data from 20 consecutive patients who underwent maxillary orthognathic surgery through a Le Fort I osteotomy for advancement and/or superior repositioning was analyzed. All patients had an incision from canine-to-canine region to perform a Le Fort I osteotomy. Virtual surgical plan and development of a patient-specific reduced-size cutting guide and fixation with 2 patient-specific plates on the anterior maxilla was designed. Full-face cone-beam computer tomography (CBCTs) were obtained on the same machine (Planmeca Viso G7) before surgery and up to 7 days after surgery. The STL file of a composite skull of the virtual surgical plan was provided by the company utilized (DePuy Synthes Johnson & Johnson). The STL of the planned movements was superimposed on the immediate post-operatory CBCT at the cranial base and skull structures, using Dolphin Imaging's software 3D superimposition module. Maxillary central incisors (right and left) and second molar (right and left) points were defined. Points U1R, U1L, U7R and U7L in the plan and immediate postoperative images were directly compared in the horizontal, vertical, and transverse dimensions, in the axial, coronal, and sagittal slices. U1R and U1L had a maximum deviation of 0.5 mm in the Vertical and Horizontal dimensions, between the planned and the achieved position. U7R and U7L had a maximum of 1 mm deviation in the Vertical dimension in 2 out of 20 cases, 0.5 mm maximum deviation in the transverse position, and 0.5 mm in the Antero-posterior dimension. Overall, the average deviation of maxillary repositioning was 0.15 mm for the incisors in all dimensions and 0.25 mm for the molars in all dimensions. The larger deviation was on the vertical position of the maxillary second molar (1 mm), in 5 out of 20 cases. The results of this study show that reduced-size custom guides and plates provide accurate 3D repositioning of the maxilla ( < 0.5 mm average deviation). There was no correlation between magnitude and type of maxillary movement and the accuracy. Positioning of the guide and plates can be accomplished with a reduced invasiveness approach. Long-term outcomes are needed to assess maxillary stability with a 2-plate fixation method.Jones, J. P., Amarista, F. J., Jeske, N. A., Szalay, D. & Ellis, E. Comparison of the Accuracy of Maxillary Positioning With Interim Splints Versus Patient-Specific Guides and Plates in Executing a Virtual Bimaxillary Surgical Plan. J Oral Maxil Surg 80, 827–837 (2022).Al Asseri, N. & Swennen, G. Minimally invasive orthognathic surgery: a systematic review. Int J Oral Max Surg 47, 1299–1310 (2018).
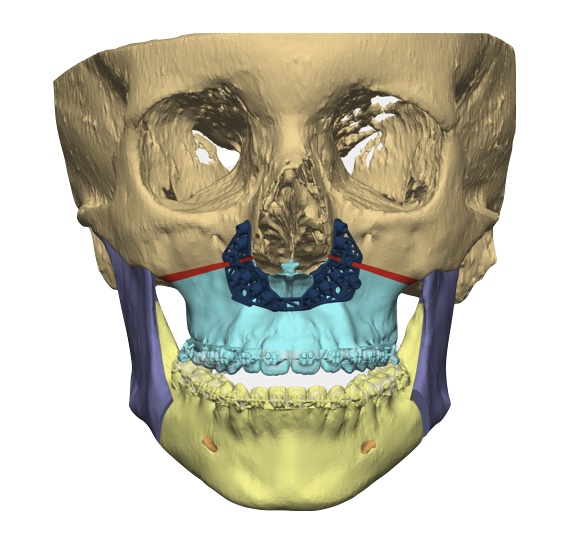
Custom Cutting Guide Design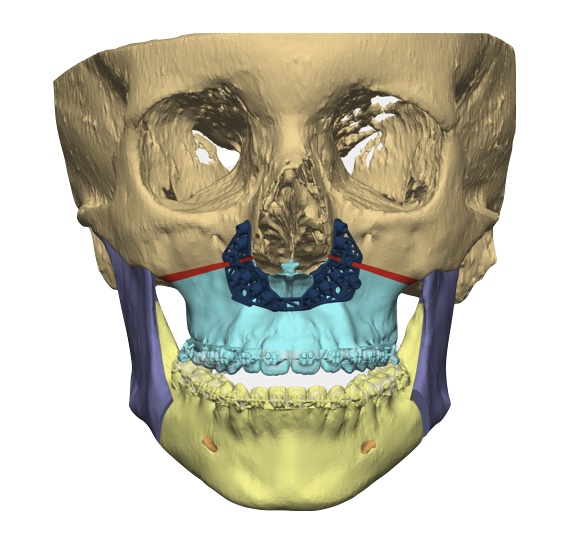
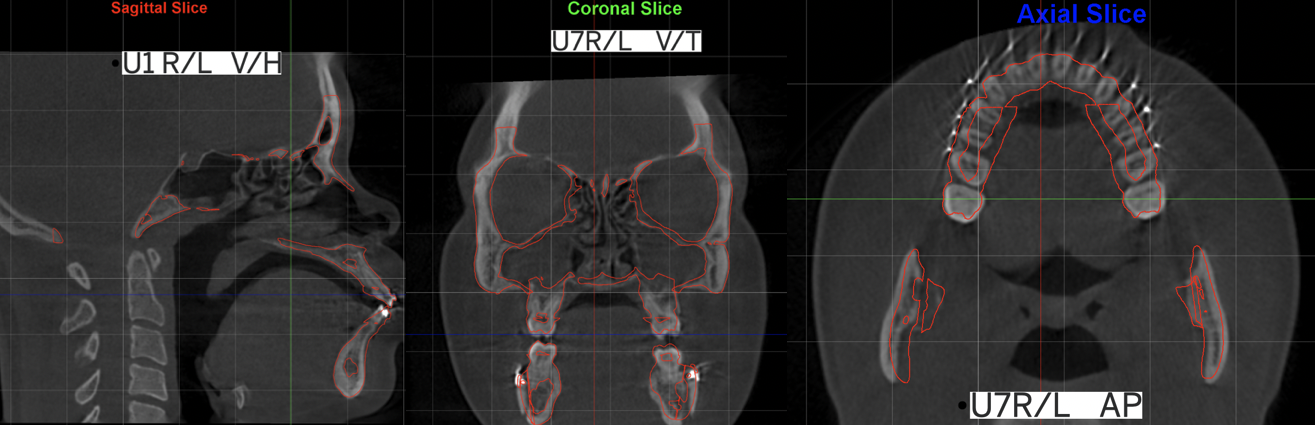
Superimposition immediate postop CBCT and STL of VSP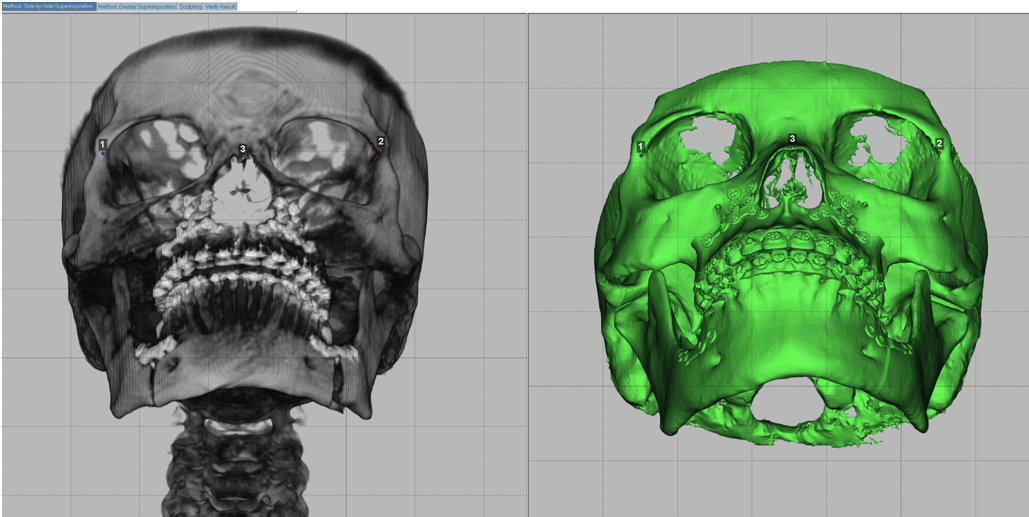
Red lines show VSP over postop CBCT, measured in 3 dimensions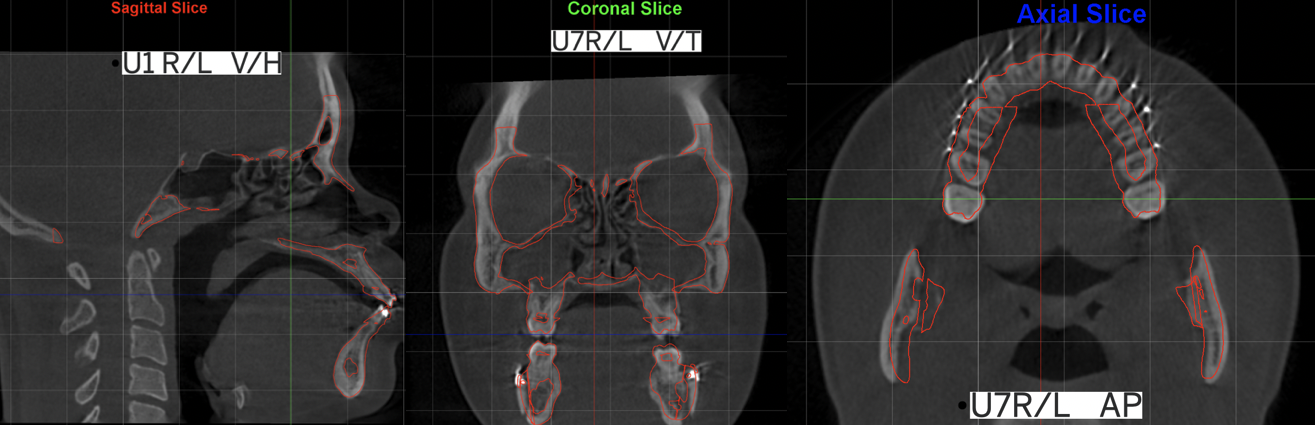
Custom Cutting Guide Design
Superimposition immediate postop CBCT and STL of VSP
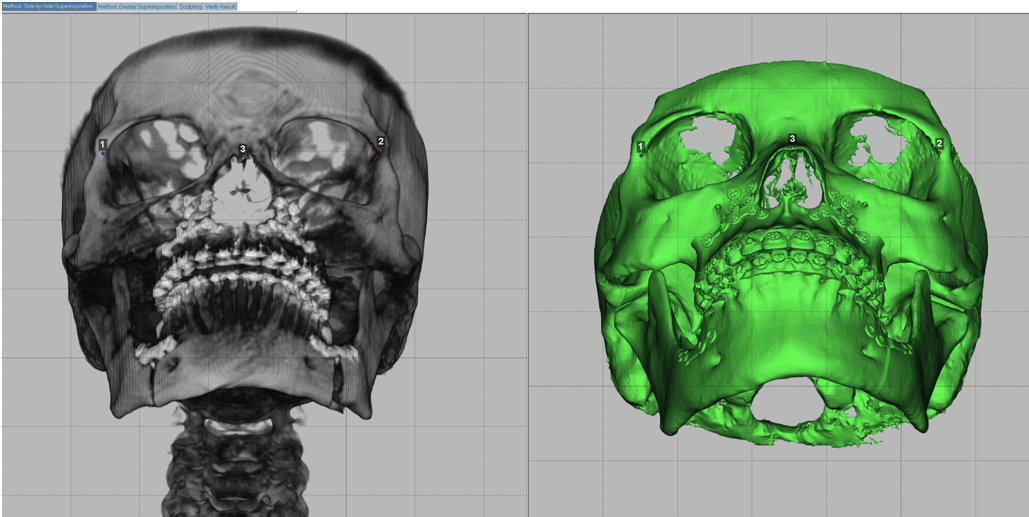
Red lines show VSP over postop CBCT, measured in 3 dimensions