Dental Implants
OMS and Other Dental Specialists
Session: Oral Abstract Session Three
SA3 - Endoscopy Mediated Sinus Augmentation (EMS): Retrospective 10-Case Series of a Novel Technique
Saturday, September 14, 2024
8:30 AM - 8:40 AM EDT
Location: W315B, Orange County Convention Center

Pooria Fallah Abed, DDS
Periodontist
Modern Perio Implant
Dallas, Texas
Oral Abstract Presenter(s)
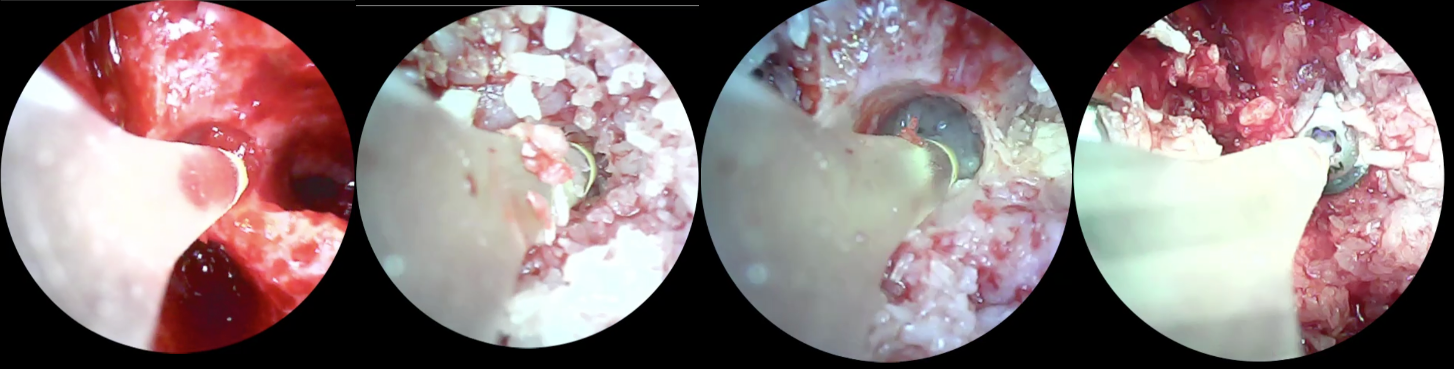
Abstract: Various techniques for sinus augmentation in atrophic posterior maxilla pose challenges due to their lack of visual feedback. Sinus perforation, a common complication during lateral window and crestal approaches, results from poor visibility. Improving visibility can enhance predictability, reduce complications, and offer a less invasive option. Previous attempts of using endoscope were not successful due to the technical difficulties.In this novel approach an Endoscopic camera with a 4.0 mm diameter (1080 HD screen, LED light) was used in ten patients. EMS is equipped with a wireless camera with recording capability. The anticorrosive and water-resistant feature of the camera makes it possible to withstand cold sterile sterilization. Different tips of sinus augmentation instruments have been modified then attached to the camera. When faced with residual bone measuring less than 4 mm due to the narrow diameter of the camera and instrument tip following the completion of a 3.5 mm or larger osteotomy during implant site preparation, a specialized instrument tip was employed to initiate the lift. After completing the lift, a different instrument tip was used for the precise delivery of allograft particulate cortical and cancellous bone graft material. This step was followed by implant placement and the camera was used for monitoring throughout the procedure. The instrument and camera together are used by the clinician during the procedure to keep better visibility during the lift, in both lateral and crestal approach. CBCTs were used preoperatively and 6-month post operatively to measure residual bone height (RBH), Bone height gain (BHG), peri implant bone loss (PIB), and bone density at mid length. Patient satisfaction was measured with a visual analog scale (VAS).In a seven-month study, 11 implants in 10 patients showed successful placement with primary stability, and no failures were observed. VAS pain scores decreased gradually, averaging 2.0 at 24 hours and 0.6 at 2 weeks post-surgery. RBH measured 3.1 mm, with an average BHG of 8.7 mm. Definitive restoration occurred between 5 to 7 months. PIB was minimal at 0.3 mm. The camera identified three small perforations (27%) during sinus augmentation, which were all successfully repaired. This perforation rate is notably lower than the previously reported 53.8% (residual bone < 5 mm) without direct vision. EMS ensured direct visual feedback, and no issues with inadequate or uneven distribution of bone graft materials were observed. The picture illustrates the osteotomy and Schneiderian membrane visibility with a minimally invasive approach at the crest and no vertical incisions followed step by step by step of using EMS until implant placement. In contrast to the traditional sinus augmentation technique, which necessitates an extensive incision for access in the lateral window approach, this technique allows for clear visibility during the initial lift. If the lateral window approach remains the preferred method, it still effectively minimizes the size of the window. EMS has streamlined the lift process, providing a clearer illustration of the anatomy and direct vision through the high-definition camera. The device was inserted deeper into the sinus to achieve complete elevation of the membrane from the sinus floor and all surrounding walls, especially the medial wall, where visibility is difficult often constituting a "blind spot.The EMS technique focuses on minimally invasive sinus augmentation in an atrophic posterior maxilla, providing direct visibility for clinicians, and thus better clinical judgement, for both crestal and lateral window approaches. With as little as 2 mm residual bone, it opts for complete sinus augmentation through an osteotomy, reducing complications during implant placement and post operatively. The direct visual feedback improves clinical outcomes while also enhancing the patient experience.
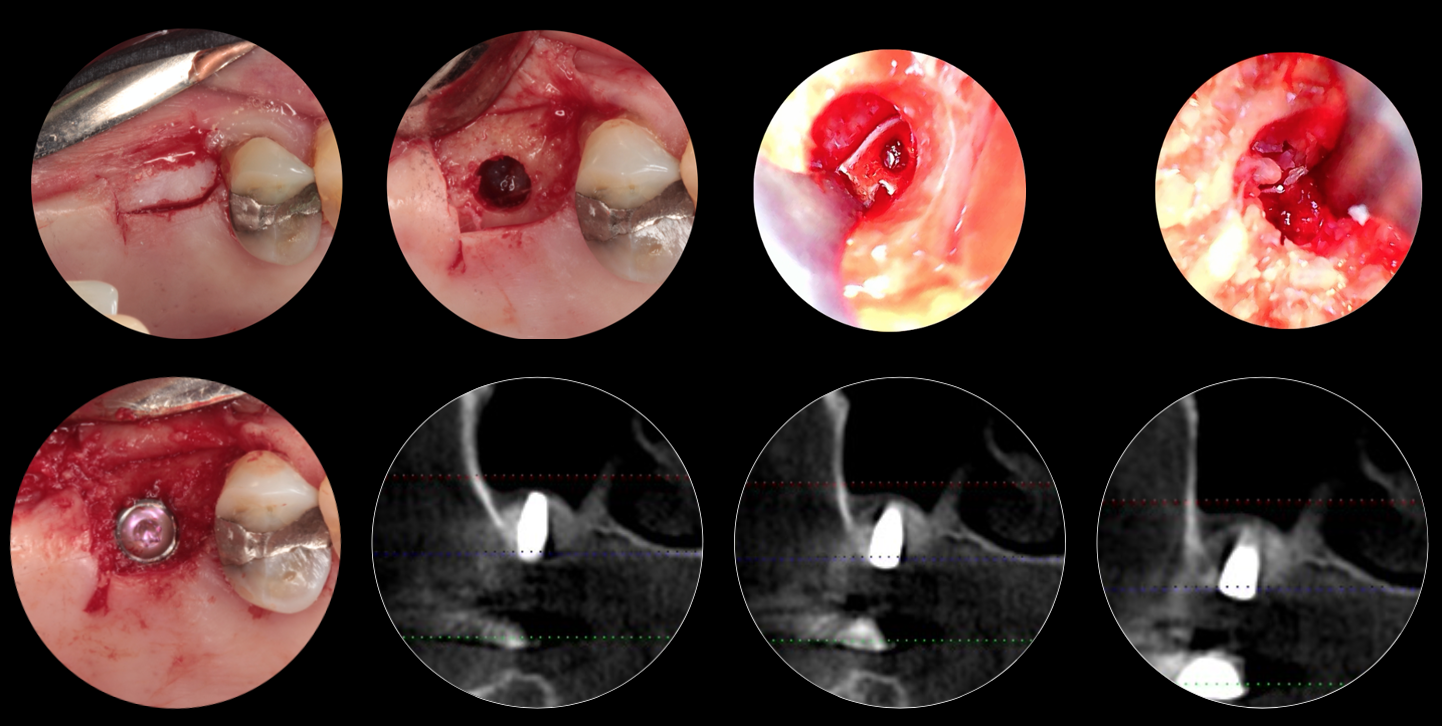
EMS for augmentation site #14 after extraction followed by implant placement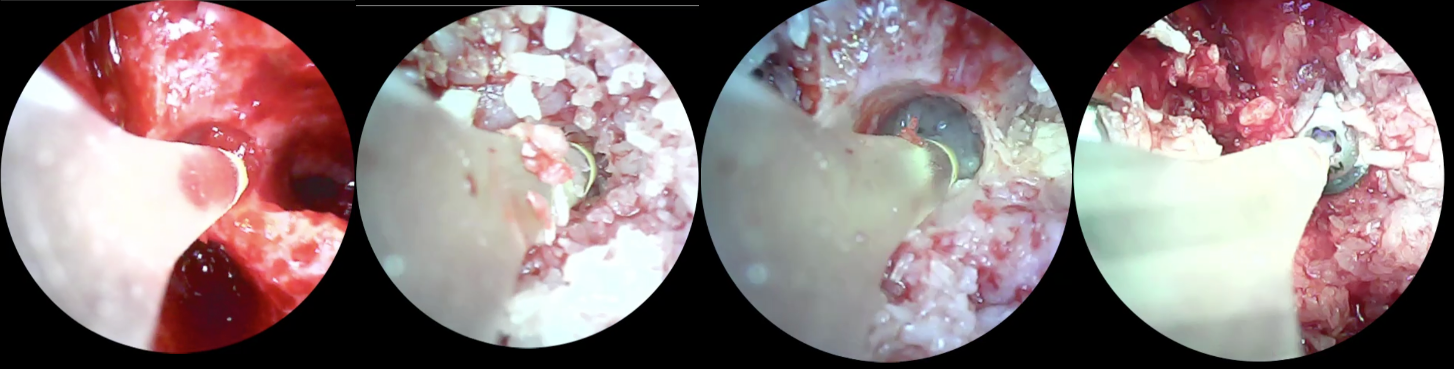
EMS for augmentation of site 3 with minimal residual bone, Minimal invasive to avoided extensive lateral window approach, Post Operative CBCT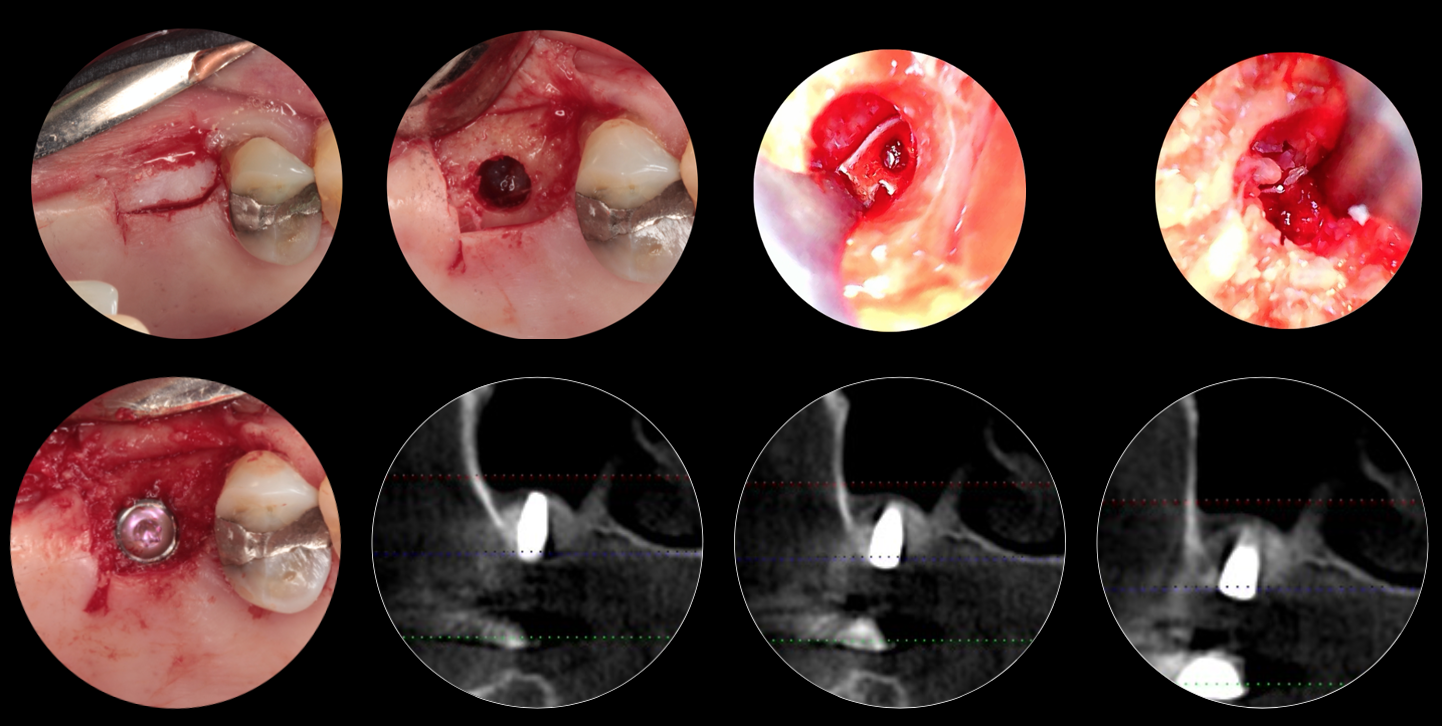
EMS for augmentation site #14 after extraction followed by implant placement
EMS for augmentation of site 3 with minimal residual bone, Minimal invasive to avoided extensive lateral window approach, Post Operative CBCT